Navigating the Skin Changes of Menopause: A Guide to Managing Menopausal Acne
Related Articles: Navigating the Skin Changes of Menopause: A Guide to Managing Menopausal Acne
Introduction
With enthusiasm, let’s navigate through the intriguing topic related to Navigating the Skin Changes of Menopause: A Guide to Managing Menopausal Acne. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Navigating the Skin Changes of Menopause: A Guide to Managing Menopausal Acne
Menopause, a natural transition in a woman’s life, often brings about a cascade of hormonal shifts that can significantly impact skin health. One of the most unwelcome and perplexing changes is the emergence or worsening of acne, a condition commonly referred to as menopausal acne. While acne is typically associated with adolescence, the hormonal fluctuations during menopause can trigger similar inflammatory responses in the skin, leading to breakouts.
This article delves into the complex interplay between menopause and acne, providing a comprehensive guide to understanding, managing, and mitigating this skin concern. It explores the underlying causes, examines effective skincare practices, and offers insights into treatment options available to address menopausal acne.
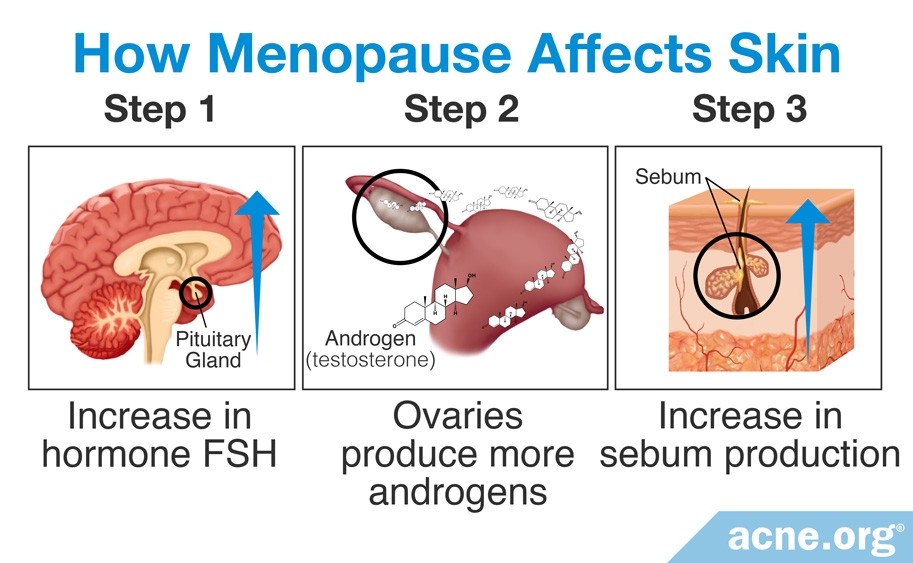
Understanding the Hormonal Connection
Menopause marks the end of menstruation, signifying a decline in estrogen production. Estrogen plays a crucial role in regulating sebum production, a natural oil that lubricates the skin. With reduced estrogen levels, the skin’s oil glands can become overactive, leading to increased sebum secretion. This excess oil can clog pores, creating a fertile ground for bacteria to proliferate, ultimately resulting in acne breakouts.
Furthermore, the decline in estrogen can disrupt the skin’s natural barrier function, making it more susceptible to irritation, inflammation, and breakouts. The skin’s ability to retain moisture is also compromised, contributing to dryness and a heightened sensitivity to environmental factors.
The Impact of Other Hormonal Changes
While estrogen is the most prominent hormone involved in menopausal acne, other hormonal shifts contribute to the condition. The reduction in progesterone, another female sex hormone, can also impact sebum production and skin cell turnover. Additionally, an increase in androgen levels, primarily testosterone, can stimulate oil gland activity and exacerbate acne.
Beyond Hormones: Other Contributing Factors
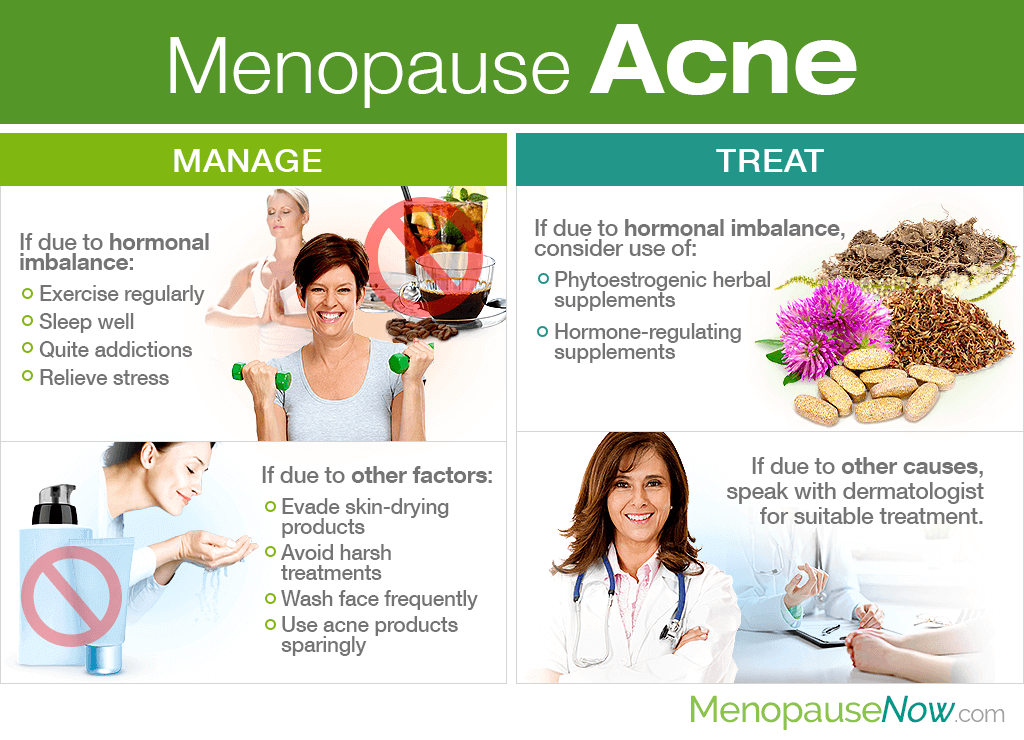
While hormonal fluctuations are the primary drivers of menopausal acne, other factors can exacerbate the condition:
- Stress: Stress can disrupt hormonal balance, leading to an increase in cortisol, a stress hormone that can trigger inflammation and worsen acne.
- Diet: A diet rich in processed foods, sugary drinks, and unhealthy fats can contribute to inflammation and exacerbate acne.
- Medications: Certain medications, including corticosteroids and some anticonvulsants, can trigger acne as a side effect.
- Skincare Products: Harsh cleansers, heavy moisturizers, and comedogenic (pore-clogging) ingredients can contribute to acne formation.
Navigating the Skincare Routine: A Holistic Approach
Managing menopausal acne requires a multi-pronged approach, incorporating a tailored skincare routine, lifestyle adjustments, and, in some cases, medical treatments.
1. Gentle Cleansing:
The foundation of any effective skincare routine is a gentle cleansing regimen. Opt for a mild, non-comedogenic cleanser formulated for sensitive skin. Avoid harsh soaps, scrubs, or alcohol-based products that can strip the skin of its natural oils and exacerbate dryness.
2. Exfoliation:
Regular exfoliation helps remove dead skin cells, unclog pores, and prevent breakouts. However, it is crucial to choose a gentle exfoliating agent, such as a chemical exfoliant containing salicylic acid or glycolic acid. Avoid harsh physical scrubs that can irritate the delicate skin.
3. Targeted Treatments:
For active acne lesions, incorporate spot treatments containing benzoyl peroxide or salicylic acid. These ingredients effectively kill bacteria, reduce inflammation, and promote healing.
4. Moisturizing:
Despite the increased sebum production, menopausal skin can become dry and dehydrated. It is essential to moisturize regularly with a lightweight, non-comedogenic moisturizer. Look for products enriched with hyaluronic acid, ceramides, or other hydrating ingredients.
5. Sun Protection:
Sun exposure can worsen acne and accelerate skin aging. Always apply a broad-spectrum sunscreen with an SPF of 30 or higher, even on cloudy days.
6. Lifestyle Modifications:
Alongside skincare practices, lifestyle changes can significantly impact acne management:
- Stress Management: Engage in stress-reducing activities like yoga, meditation, or spending time in nature.
- Dietary Changes: Limit processed foods, sugary drinks, and unhealthy fats. Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
- Hydration: Drink plenty of water throughout the day to keep the skin hydrated and flushed of toxins.
- Sleep: Aim for 7-8 hours of quality sleep each night to allow the body to repair and rejuvenate.
Seeking Professional Guidance
For persistent or severe acne, consulting a dermatologist is highly recommended. They can assess the underlying causes, recommend personalized treatment plans, and offer guidance on managing menopausal skin changes.
Treatment Options for Menopausal Acne
A dermatologist may recommend various treatment options, including:
- Topical Medications: Retinoids, topical antibiotics, and anti-inflammatory agents can effectively treat acne.
- Oral Medications: In some cases, oral antibiotics or hormonal therapies may be prescribed.
- Light Therapy: Blue light therapy can kill acne-causing bacteria.
- Chemical Peels: Chemical peels can remove dead skin cells, unclog pores, and promote collagen production.
Frequently Asked Questions
1. What is the best way to prevent menopausal acne?
The best way to prevent menopausal acne is to adopt a holistic approach that includes:
- Maintaining a healthy lifestyle with a balanced diet, regular exercise, and adequate sleep.
- Managing stress levels through relaxation techniques.
- Practicing a gentle, non-comedogenic skincare routine.
- Consulting a dermatologist for personalized advice and treatment options.
2. Can I use over-the-counter acne products for menopausal acne?
Over-the-counter acne products can be effective for mild cases of menopausal acne. However, it’s crucial to choose products formulated for sensitive skin and avoid harsh ingredients. Consulting a dermatologist can help determine the most appropriate products for your specific needs.
3. How long does it take to see results from treatment?
The time it takes to see results from acne treatment varies depending on the severity of the condition and the chosen treatment method. Topical treatments may show improvement within a few weeks, while oral medications or more invasive treatments may require several months to achieve optimal results.
4. Can menopausal acne be cured?
While menopausal acne cannot be cured, it can be effectively managed with a combination of skincare practices, lifestyle modifications, and, in some cases, medical treatments. The goal is to minimize breakouts, improve skin clarity, and maintain a healthy, radiant complexion.
5. Can I use makeup on my acne-prone skin?
It is generally safe to use makeup on acne-prone skin, but it’s important to choose non-comedogenic, oil-free products. Opt for mineral makeup, which is less likely to clog pores. Avoid heavy foundations and concealers that can trap oil and bacteria.
Tips for Managing Menopausal Acne
- Cleanse twice daily: Wash your face twice a day with a gentle, non-comedogenic cleanser.
- Exfoliate 1-2 times a week: Use a chemical exfoliant with salicylic acid or glycolic acid to remove dead skin cells and unclog pores.
- Moisturize regularly: Apply a lightweight, non-comedogenic moisturizer to keep the skin hydrated.
- Use spot treatments: Apply benzoyl peroxide or salicylic acid spot treatments to active acne lesions.
- Wear sunscreen daily: Protect your skin from the sun with a broad-spectrum sunscreen with an SPF of 30 or higher.
- Manage stress: Engage in stress-reducing activities like yoga, meditation, or spending time in nature.
- Eat a healthy diet: Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
- Drink plenty of water: Stay hydrated by drinking plenty of water throughout the day.
- Get enough sleep: Aim for 7-8 hours of quality sleep each night.
- Consult a dermatologist: Seek professional advice for persistent or severe acne.
Conclusion
Menopausal acne is a common skin concern that can be effectively managed with a comprehensive approach. Understanding the hormonal shifts associated with menopause, adopting a tailored skincare routine, making lifestyle modifications, and seeking professional guidance from a dermatologist are crucial steps in achieving clear, healthy skin during this life transition. By embracing these strategies, women can navigate the skin changes of menopause with confidence and maintain a radiant complexion.







Closure
Thus, we hope this article has provided valuable insights into Navigating the Skin Changes of Menopause: A Guide to Managing Menopausal Acne. We appreciate your attention to our article. See you in our next article!